Blood transiently shifted by the human diving response could cause SUDEP
Pulmonary edema occurs when the fluid inside pulmonary capillaries leaks into, or through, the capillary-alveolar membrane. When this occurs, gas exchange between alveoli and red blood cells is hindered, or blocked altogether, resulting in low blood oxygen levels.
Several studies show that convulsive seizures often cause pulmonary edema. It is not known why this happens but this transient form of edema can be instantly precipitated by a greater than normal rush of blood through the pulmonary capillaries. As the mammalian dive (or diving) response (MDR) causes a rapid, and transient, shift of the body’s blood into the pulmonary circulation, it is possible that seizure-induced pulmonary edema, and subsequent death, is explained by the MDR.
Watch the video.
Can the risk of death from a seizure (SUDEP) be predicted?
At any given time, over 60% of the body’s circulating polymorphonucleocytes (a type of immune cell that includes neutrophils, basophils, eosinophils and MAST cells) are in transit through the lungs. But when pulmonary blood flow increases, as it happens when people exercise, become anxious, or have a seizure, these immune cells are propelled back into the peripheral blood and cause a detectable elevation of the white blood cell count. Could the blood shift of the mammalian diving response, which fuels a major increase in pulmonary blood flow, explain the transient elevations of the white blood cell count in some epilepsy patients? If so, could this help to quantify the risk of death from seizures?
Circulating immune cells and lung blood flow during deadly seizures
Some epileptic convulsions elevate the white blood cell count. Others don’t. No one knows why. But several studies show that the magnitude of these elevations relate to patients’ clinical outcomes. Recent work even suggests they are linked to the degree of breathing abnormalities developed during or after convulsions. Could the white blood cell count be used as a harbinger of dangerously increased pulmonary blood flow, and thus of dangerously increased pressure in the pulmonary capillaries during epileptic convulsions? Could this phenomenon be related to seizure-induced mammalian diving responses?
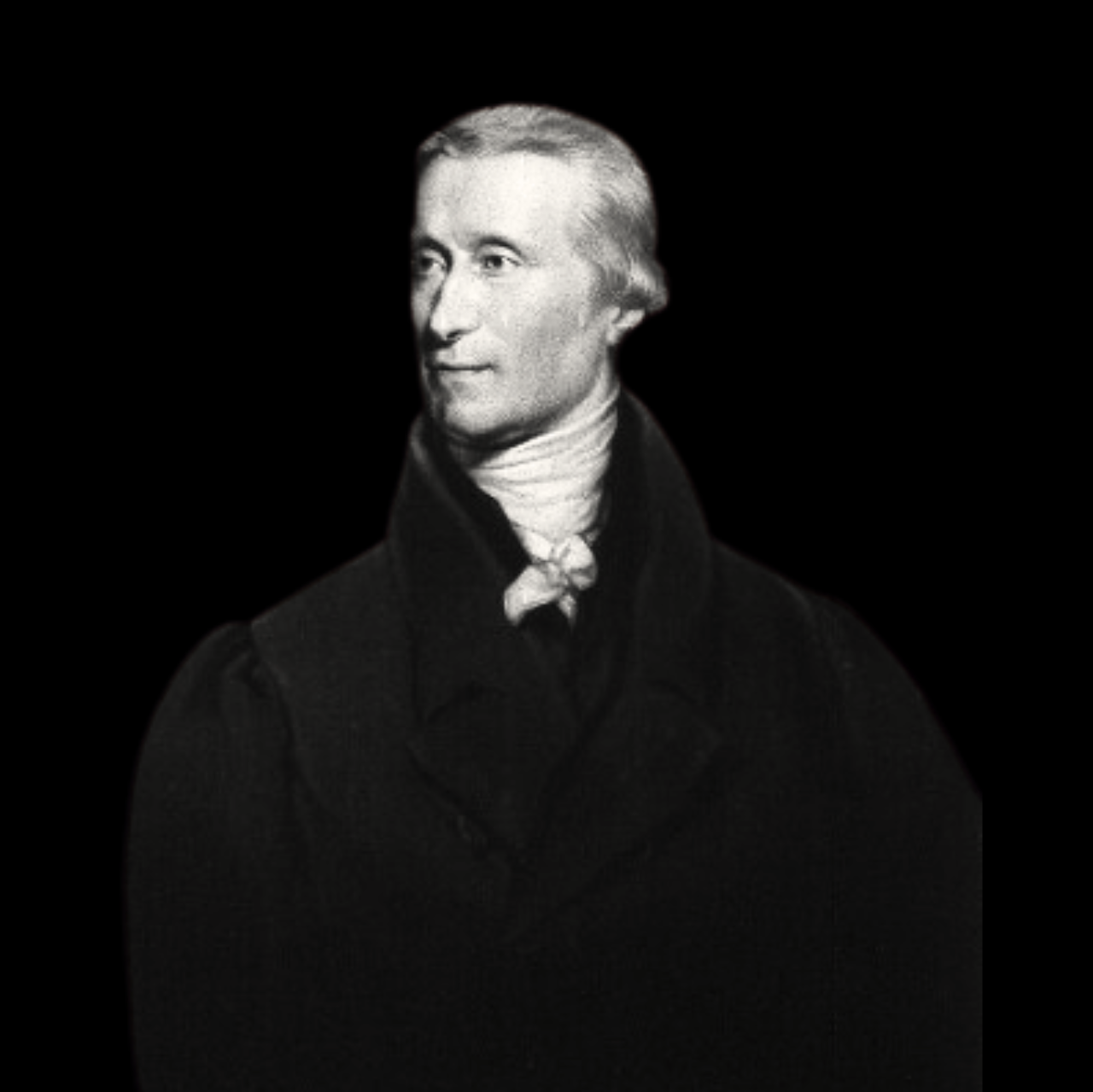
The father of the mammalian diving response was lost for over 200 years!
The science behind the mammalian diving response originated with the discovery of diving bradycardia, a primordial oxygen-conserving reflex by which the heart rate of air-breathing vertebrates, including humans, slows down in response to prolonged breathing cessation (i.e., apnea). Curiously, luminaries in the field erroneously attributed its discovery to a famous French physician, Paul Bert, even though his experiments were neither intended nor adequate for such a discovery. Instead, diving bradycardia had been described in the doctoral thesis of a little known British medical student (Edmund Goodwyn) almost 100 years before Bert’s work was published. Ironically, this student’s thesis had been appropriately referenced, for all to see, in Bert’s own list of citations.